The Food and Drug Administration (FDA) has updated the information in its Frequently Asked Questions (FAQs) regarding diagnostic devices for COVID-19, including 3D printed swabs.
The Administration ultimately intends to decline reviews of emergency use authorization (EUA) requests when it comes to laboratory developed tests (LDTs). The announcement comes following a release by the US Department of Health and Human Services stating that novel LDTs would not be subjected to premarket review.

Increasing U.S. testing capabilities
While the FDA will no longer accept EUAs for LDTs, it will still continue to review requests for point-of-care tests, home collection tests, and any other tests that may alleviate national shortages. This includes high-throughput, widely distributed tests, as the Administration hopes to increase the country’s overall testing capacity and accessibility.
The FDA stated: “We are currently in a different phase of the pandemic with respect to tests than we were previously, where many COVID-19 tests are now authorized to be run in labs. We prioritize review of EUA requests for tests taking into account a variety of factors, including those discussed in the Emergency Use Authorization of Medical Products and Related Authorities Guidance, such as the public health need for the product and the availability of the product.”
Updates on 3D printed swabs
Within the new FAQs, the FDA has advised on which specimen types can be swab tested. As it stands, this includes nasopharyngeal, oropharyngeal, mid-turbinate and anterior nares specimens. The Administration also provides guidance on the proper method of collecting these specimens, as poor swabbing techniques can result in inadequate samples and injuries.
When it comes to 3D printed swabs, which are Class I medical devices, the new guidance states that sterile swabs that do not require premarket notification will not need an EUA for distribution to occur. Any and all facilities that manufacture these sterile swabs must, however, register and list their additively manufactured products. The swabs must also meet any applicable medical device regulatory requirements, such as those related to quality systems and reports of corrections.
The FDA adds: “As a general matter, 3D printing can introduce certain challenges not seen with conventional manufacturing. FDA is aware that some users have reported concerns of brittle 3D printed swabs that have broken into multiple sharp pieces, and non-traditional capture geometries that may not capture the sample sufficiently. While FDA and the clinical community have vast experience with traditional swabs, there is limited prior experience with the use of 3D printed swabs for specimen collection for diagnostic testing.”
Prior to the FDA update, global certification firm TÜV SÜD provided a set of 3D printing standards and regulations checklists for manufacturers producing COVID-19-related medical devices. In line with the FDA, the checklists are intended to ensure the products adhere to the strict quality requirements and legal regulations medical devices are usually subject to.
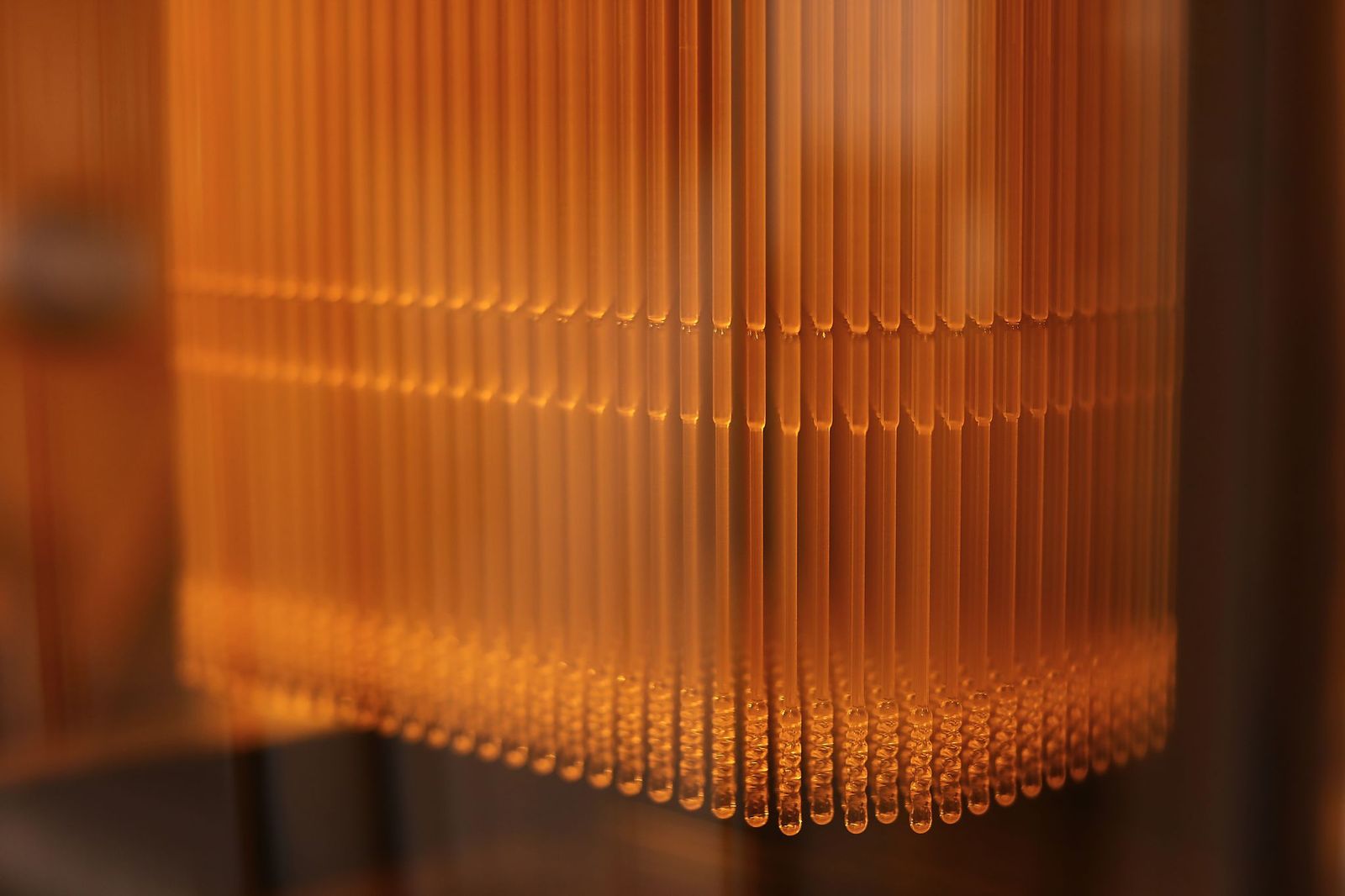
Elsewhere, 3D printing service bureau PrintParts recently partnered with post-processing system developer PostProcess Technologies to additively manufacture nasal swabs in New York City. The parts, specifically, are designed to collect nasopharyngeal specimens and are made of a translucent photopolymer resin.
Subscribe to the 3D Printing Industry newsletter for the latest news in additive manufacturing. You can also stay connected by following us on Twitter and liking us on Facebook.
Looking for a career in additive manufacturing? Visit 3D Printing Jobs for a selection of roles in the industry.
Featured image shows 3D printed nasal swabs from the University of South Florida Health. Photo via USF Health.



