Nominations for the 2024 3D Printing Industry Awards are now open. Tell us who is leading.
Researchers at Harvard’s Wyss Institute for Biologically Inspired Engineering and the John A. Paulson School of Engineering and Applied Science (SEAS) have developed a novel method for 3D printing vascular networks that could advance the field of organ transplantation.
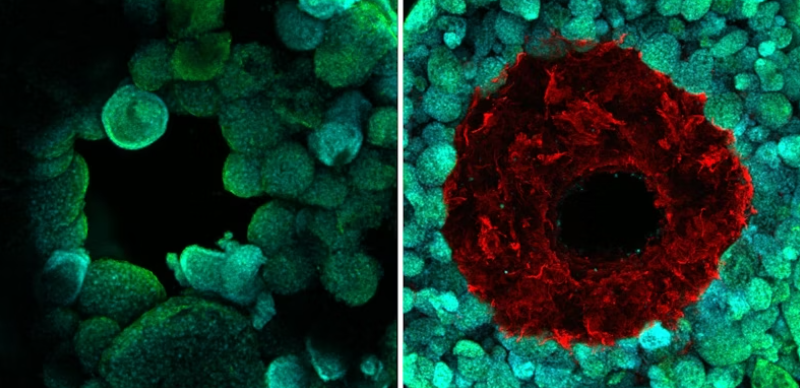
Focused on creating functional human organs outside the body, this new technique features a design that mimics the structure of natural blood vessels. Developed from a previous method called sacrificial writing in functional tissue, this new method named coaxial SWIFT (co-SWIFT) enables the creation of interconnected networks of blood vessels embedded within human cardiac tissue, enhancing the viability of producing implantable human organs.
Published in Advanced Materials, this study was supported by grants from the Vannevar Bush Faculty Fellowship and the National Science Foundation, with contributions from a team of researchers including Katharina Kroll, Alexander Ainscough, Daniel Reynolds, Alexander Elamine, Ben Fichtenkort, and Sebastien Uzel as co-authors.
“To say that engineering functional living human tissues in the lab is difficult is an understatement. I’m proud of the determination and creativity this team showed in proving that they could indeed build better blood vessels within living, beating human cardiac tissues. I look forward to their continued success on their quest to one-day implant lab-grown tissue into patients,” said Wyss Founding Director Donald Ingber, M.D., Ph.D.
3D printing biomimetic blood vessels
For this approach, the team used a core-shell nozzle designed for 3D printing, which allows for the construction of blood vessels with a shell of smooth muscle cells and endothelial cells around a hollow core through which fluids can flow.
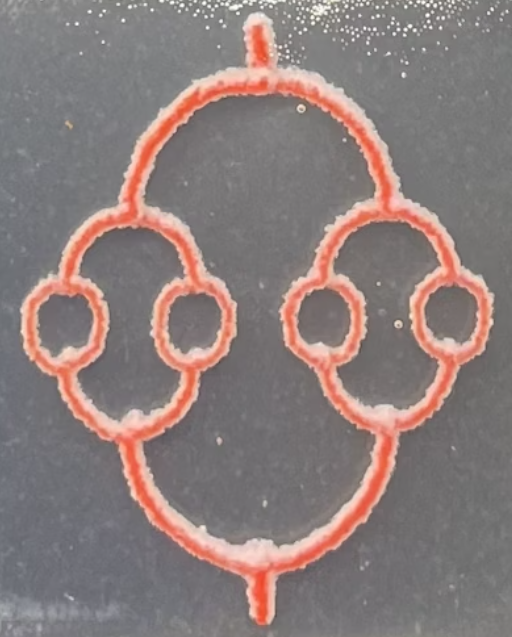
The process initiated by the team involves two unique “inks” to create the vessels: a collagen-based shell ink for constructing the vessel walls and a gelatin-based core ink for forming the hollow center. By adjusting the printing speed and ink flow rate, the researchers tailored the size of the vessels. After printing, these structures are embedded into either a hydrogel matrix or a novel porous collagen-based material known as uPOROS, replicating muscle tissue properties.
This was followed by the team heating the matrix, causing the collagen to crosslink and the gelatin core to melt away, leaving behind a perfusable vascular network. According to the researchers, this step is crucial for the formation of open and functional blood vessels.
Enhancing the biomimetic quality of the printed vessels, the team incorporated smooth muscle cells into the shell ink. Following the removal of the gelatin core, the team perfused endothelial cells to establish the inner layer of the blood vessels. Subsequent tests confirmed that these cells stayed viable and functional, markedly decreasing the vessels’ permeability compared to those lacking an endothelial lining.
Once integrated into dense matrices of cardiac cells, the vascular structures began beating synchronously when perfused with a blood-mimicking fluid, showcasing the functionality of these 3D printed tissues as healthy and functional heart tissue. Additionally, these tissues responded correctly to drugs affecting heart rate, demonstrating their potential in drug testing and disease modeling.
This research advances organ transplantation development and demonstrates the creation of patient-specific tissues, as noted from a printed model of a patient’s coronary artery. Future plans for this technology include developing networks of capillaries to enhance the functionality of lab-grown tissues, moving closer to the goal of replicating the full structure of human blood vessels.
Tell us what you think of this 3D printing news. Make sure you click submit!
Previous developments in vascular 3D printing
3D printing vascular networks is an ongoing endeavor. Back in 2021, Scientists from the Israel Institute of Technology (Technion) used 3D printing to create a functional network of large and small blood vessels capable of supplying blood to implanted tissues.
Led by Professor Shulamit Levenberg, this research aimed to bypass the need for pre-transplant steps and reduce the risk of implant rejection by using patient-specific tissues. After testing the vascular network in rats, the team planned to adapt the technology for larger animals, advancing toward lab-grown tissues suitable for transplantation.
A few years before this, researchers at the University of California developed a method to 3D print functional blood vessels using hydrogel and endothelial cells. Directed by Professor Shaochen Chen, the team successfully integrated these printed vessels into the circulatory system of mice, where they merged with existing blood vessels.
While the vessels circulated blood, they were unable to transfer nutrients and waste, said the team. This research aimed to overcome a key barrier in organ transplants, with future efforts focused on patient-specific tissues and potential clinical trials.
What 3D printing trends do the industry leaders anticipate this year?
What does the Future of 3D printing hold for the next 10 years?
To stay up to date with the latest 3D printing news, don’t forget to subscribe to the 3D Printing Industry newsletter or follow us on Twitter, or like our page on Facebook.
While you’re here, why not subscribe to our Youtube channel? Featuring discussion, debriefs, video shorts, and webinar replays.
Featured image shows the original SWIFT method (left) printed hollow channels through living OBBs (green), but had no structure to contain fluid as it flowed through. Co-SWIFT (right) creates a cell-laden vessel (red) surrounding the channel, which isolates blood flow from the tissue and improves their viability. Image via Wyss Institute at Harvard University.